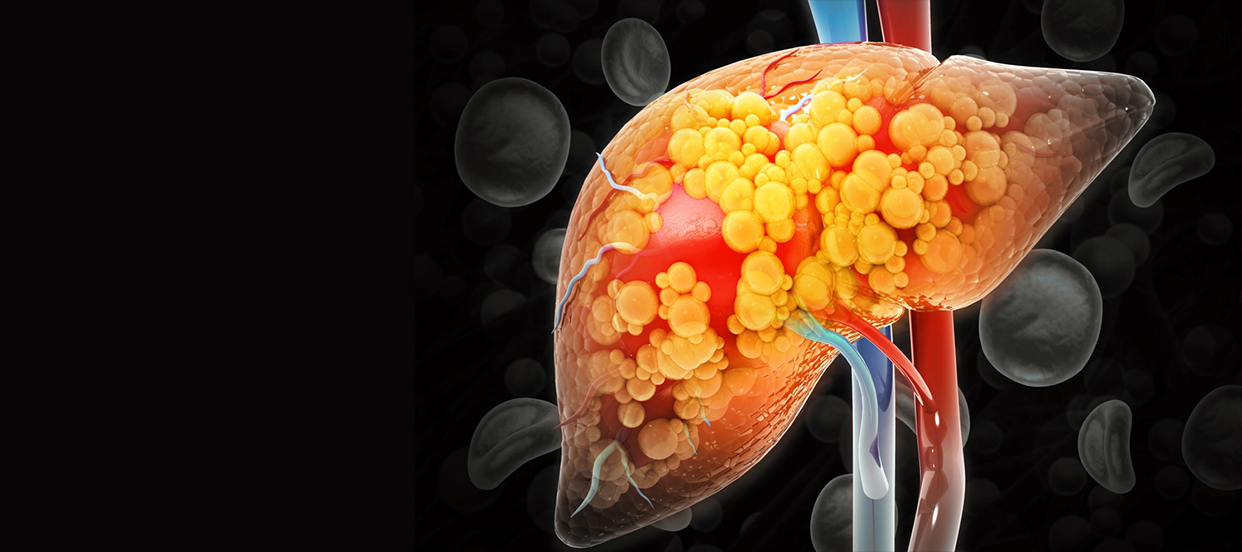
Fatty liver disease, medically known as steatotic liver disease (SLD), is a condition characterized by the accumulation of excess fat in liver cells. While it's normal for the liver to contain some fat, when fat constitutes more than 5% to 10% of the liver's weight, it is considered a fatty liver. This condition can progress through various stages, potentially leading to severe liver damage if not addressed.
Fatty liver disease encompasses a spectrum of liver conditions. The initial stage involves simple fatty liver, where fat accumulates in the liver without causing significant inflammation or damage. This stage is often benign and may not present noticeable symptoms. However, if left unmanaged, it can progress to more severe forms.
Read Also: 6 Early Signs of Liver Damage
The development of fatty liver disease is associated with several factors. Obesity is a primary contributor, as excess body weight leads to fat accumulation in the liver. Insulin resistance, commonly seen in individuals with type 2 diabetes, causes elevated blood sugar levels, which can increase fat storage in the liver. High cholesterol and triglyceride levels also contribute to fat buildup.
Metabolic syndrome, a cluster of conditions including increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels raises the risk of developing fatty liver disease. Genetic factors may also play a role, making some individuals more susceptible to fat accumulation in the liver.
Read Also: What is Grade 2 Fatty Liver? Symptoms, Causes and Treatment
In its early stages, fatty liver disease often presents no noticeable symptoms, making it challenging to detect without medical testing. As the condition progresses, individuals may experience persistent fatigue, discomfort or pain in the upper right abdomen, and unexplained weight loss. Some may notice weakness or a general feeling of being unwell. In advanced stages, symptoms can include jaundice (yellowing of the skin and eyes), swelling in the abdomen and legs, and mental confusion, indicating significant liver impairment.
Read Also: Fatty Liver Grade 3: Symptoms, Causes And Treatment
Fatty liver disease progresses through several stages. The initial stage, known as simple fatty liver or steatosis, involves fat accumulation without significant inflammation. If unmanaged, it can advance to nonalcoholic steatohepatitis (NASH), characterized by liver inflammation and damage. Persistent inflammation leads to fibrosis, where scar tissue forms in the liver. Over time, extensive scarring can result in cirrhosis, severely impairing liver function and potentially leading to liver failure or liver cancer.
Read Also: 7-Day Indian Meal Plan for Fatty Liver Disease
Diagnosing fatty liver disease typically involves a combination of medical history evaluation, physical examination, and diagnostic tests. Blood tests can assess liver function and detect elevated liver enzymes, indicating liver inflammation. Imaging studies, such as ultrasound, CT scans, or MRI, can visualize fat accumulation in the liver. In some cases, a liver biopsy may be performed to assess the extent of liver damage and rule out other conditions.
Managing fatty liver disease primarily focuses on lifestyle modifications. Weight loss through a combination of a healthy diet and regular exercise is crucial, as it can reduce liver fat and inflammation. Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins while limiting saturated fats, refined carbohydrates, and sugars is beneficial. Regular physical activity, such as aerobic exercises and strength training, enhances insulin sensitivity and promotes weight loss. Controlling blood sugar levels and managing cholesterol through diet, exercise, and medications if necessary are also important. Avoiding alcohol is essential, as it can exacerbate liver damage. In some cases, medications may be prescribed to manage underlying conditions like diabetes or to reduce liver inflammation.
Preventing fatty liver disease involves maintaining a healthy lifestyle. This includes achieving and sustaining a healthy weight through a balanced diet and regular exercise. Limiting alcohol consumption and avoiding excessive intake of sugary and fatty foods are also important preventive measures. Regular medical check-ups can help monitor liver health and detect early signs of liver disease, allowing for timely intervention.
Fatty liver disease is a progressive condition that can lead to serious liver complications if not addressed. Understanding its causes, recognizing the symptoms, and implementing preventive measures are crucial steps in managing and preventing the progression of this disease. By adopting a healthy lifestyle and seeking regular medical care, individuals can significantly reduce their risk of developing fatty liver disease and its associated complications.
Q1: Is fatty liver serious?
A: It can be. In its early stages, it's often harmless. But if it's not managed, it can worsen over time, leading to serious liver damage like cirrhosis or even liver failure.
Q2: How common is fatty liver?
A: It's estimated that a significant portion of adults have some degree of fatty liver, especially with the rise in obesity and related conditions.
Q3: Am I at risk for fatty liver if I'm not overweight?
A: While obesity is a major risk factor, you can still get fatty liver even if you're at a normal weight. Other risk factors include type 2 diabetes, high cholesterol, and certain genetic conditions.
Q4: Does drinking alcohol cause fatty liver?
A: Yes, excessive alcohol consumption is a major cause of fatty liver disease (called alcoholic fatty liver disease). But you can also get it even if you don't drink much or at all (non-alcoholic fatty liver disease or NAFLD).
Q5: Is fatty liver hereditary?
A: Genetics can play a role, making some people more susceptible. However, lifestyle factors like diet and exercise play a much bigger role for most people.
Q6: How do I know if I have fatty liver?
A: In the early stages, most people don't have any symptoms. It's often discovered during routine blood tests or imaging scans for other reasons. As it progresses, you might feel tired, have pain in your upper right belly, or lose weight without trying.
Q7: What kind of tests are there for fatty liver?
A: Doctors can prescribe blood tests to check your liver enzymes. They might also order imaging tests like an ultrasound or MRI of your liver. In some cases, a liver biopsy might be needed.
Q8: What's the treatment for fatty liver?
A: For many people, lifestyle changes are the best treatment. Losing weight, eating a healthy diet, and exercising regularly can make a big difference.
Q9: What kind of diet is good for fatty liver?
A: Focus on fruits, vegetables, whole grains, and lean protein. Limit saturated and unhealthy fats, sugary drinks, and processed foods.
Q10: Can I still drink coffee if I have fatty liver?
A: Some studies suggest that coffee might actually be good for your liver, but it's best to discuss this with your doctor.